Study reveals how treatment-resistant prostate cancer provides its own hormonal fuel
Findings, in mice, suggest potential treatment strategy
 Nupam Mahajan
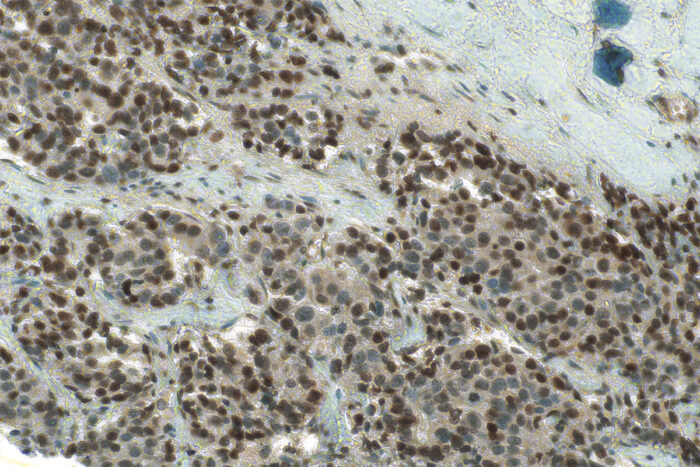
Nupam MahajanA new study from Washington University School of Medicine in St. Louis shows how prostate cancer creates its own hormonal fuel supply in response to anti-testosterone therapy. The study further suggests a strategy to block this process and potentially improve therapy options for treatment-resistant prostate cancer. Shown is a thin slice of a human prostate tumor. The dark staining throughout reveals the presence of histone acetylation promoting cholesterol production. Cholesterol is required to make testosterone, which fuels tumor growth.
A new study in mice, led by researchers at Washington University School of Medicine in St. Louis, explains how prostate cancer senses a drop in testosterone levels due to common anti-hormone therapy and then begins making cholesterol — a necessary precursor to testosterone — to generate its own testosterone to fuel tumor growth. The study also points to a possible drug combination that may stop the cancer from feeding its own growth.
Healthy prostate cells do not produce testosterone, so the research provides long-sought answers to questions about how prostate cancer cells adapt to testosterone-deprivation therapy, a common therapeutic option, by developing an ability to supply their own hormonal fuel. Further, the research reveals that treating these aggressive prostate tumors with inhibitors that block aspects of the hormonal fuel supply chain slows tumor growth in mice. These findings suggest a novel treatment strategy for prostate cancer that has become resistant to the common anti-testosterone therapy abiraterone.
The study appears June 9 in the journal Nature Communications.
The study also may help explain why Black men are at higher risk of developing prostate cancer and tend to develop more aggressive forms of the cancer than white men of European ancestry.
“We’ve known for a long time that androgens, or male hormones such as testosterone, fuel prostate tumors — and we have drugs to treat prostate cancer that block the body’s ability to make testosterone,” said senior author Nupam Mahajan, PhD, a professor of surgery in the Division of Urologic Surgery. “But after about a year, these drugs stop working, and the androgen levels rise again. Where is this androgen coming from? Turns out, prostate cancer cells have learned a new trick; they start producing more cholesterol, which they divert to generate their own androgen. Our study shows how to block this, revealing a possible drug combination that could stop prostate cancer from fueling its own growth.”
Mahajan is also a research member of Siteman Cancer Center at Barnes-Jewish Hospital and Washington University School of Medicine.
The study demonstrated how the prostate cancer cells first detect that androgen levels have dropped. The researchers found that a key protein called SREBF1, when bound to the androgen receptor, acts as an androgen sensor. When androgen levels are low, this protein enters the cancer cell nucleus, recruits an enzyme, GCN5, to modify proteins called histones through a process called acetylation. This epigenetic modification activates many genes important for manufacturing cholesterol and lipids. According to Mahajan, these two molecular events allow the cells to make enormous amounts of cholesterol, a necessary precursor for testosterone.
“The cancer cells essentially load up the tumor with cholesterol and use that cholesterol to churn out more testosterone,” Mahajan said. “That’s the trick. They overload the prostate with cholesterol, and the normal systems for making androgen from cholesterol just work as they typically would, making drugs like abiraterone ineffective.”
Mahajan and his colleagues experimented with two inhibitors that block the molecular events that they found to be responsible for the massive cholesterol manufacturing. They used these inhibitors to treat mice that had prostate tumors that had been sampled from human patients.
One drug is afatinib, an EGFR inhibitor approved by the Food and Drug Administration to treat certain types of lung cancer. The second drug is a GCN5 inhibitor. GCN5 inhibitors have not yet made it into clinical trials, but Mahajan said there is great interest in developing this class of drugs, which could have an effect on gene regulation, cell growth and inflammation. Mice treated with a combination of these two inhibitors showed large reductions in tumor volume compared with mice treated with placebo or the anti-testosterone drug abiraterone alone.
The study also suggests that the cholesterol abundance in aggressive prostate cancer may shed light on racial disparities seen in this tumor type. The researchers found evidence that the lipid profile of prostate cancer in African American men resembles the lipid profile of treatment-resistant prostate cancer identified in this study. In other words, for reasons that remain unclear, African American men with prostate cancer appear to be more prone to having an abundance of cholesterol in their tumors than white men with the same tumor type.
“This is preliminary data, so we need to verify it in larger studies,” Mahajan said. “But our study suggests that this cholesterol profile may play an important role in African American patients with prostate cancer. African American men are at higher risk of prostate cancer, are diagnosed at earlier ages, and now we see that the kinds of cholesterol molecules that are generated in their cancers are similar to what we see in this overactive cholesterol manufacturing pathway. Their cancers are more likely to already be making these lipids, even before beginning anti-testosterone treatment.”
“We are hopeful this study will provide a solid rationale for undertaking a clinical trial of these two inhibitors combined — to block this cholesterol pathway — in patients with treatment-resistant prostate cancer,” Mahajan added.






