New center to explore brain, immune system connections
Discoveries will aid efforts to develop immune therapies for neurological diseases
 Matt Miller
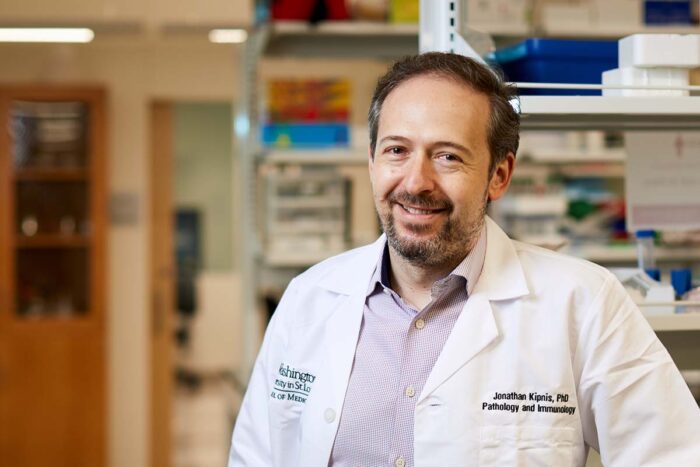
Matt MillerA new center at Washington University School of Medicine in St. Louis has been established to unravel the close connections between the brain and the immune system. The Center for Brain Immunology and Glia (BIG) will be led by Jonathan Kipnis, PhD, an international leader in the field of neuroimmunology.
As the brain reigns supreme over the human body, the immune system works 24/7 to defend the body from foreign invaders. For decades, however, the brain and the immune system were thought to operate independently of one another. But a growing body of evidence suggests the two are intimately connected in keeping the body healthy.
A new center has been established at Washington University School of Medicine in St. Louis to unravel the close connections between the brain and the immune system. Such endeavors could lead to new insight into neurological illnesses – ranging from Alzheimer’s and Parkinson’s disease to schizophrenia and autism – that are linked to an immune system gone awry, and lay the groundwork for developing promising immune-based therapies to treat such illnesses.
The Center for Brain Immunology and Glia (BIG) will be led by Jonathan Kipnis, PhD, an international leader in the new field of neuroimmunology, and the Alan A. and Edith L. Wolff Distinguished Professor. Glia are brain cells that support neurons and the myriad neural connections in the brain. They’re also involved in immune surveillance within the brain.
“Neuroimmunology is one of the most exciting areas of biomedical research,” said David H. Perlmutter, MD, executive vice chancellor for medical affairs, the George and Carol Bauer Dean of the School of Medicine, and the Spencer T. and Ann W. Olin Distinguished Professor. “The center is conceptualized to leverage the world-class programs in immunology and neurosciences that have flourished at Washington University for many years and will foster collaborations that draw established and early-career scientists from many departments and diverse disciplines to explore the two-way dialogue between the brain and the immune system.
“Such investigations are essential to designing innovative approaches to fight brain diseases and injuries,” Perlmutter added. “The center will also focus on areas that are ideal for urgently needed new therapies, so we envision that it will be a nidus for many new pharmaceutical industry partnerships. We are thrilled that Jony Kipnis is taking the helm and leading the way on this scientific journey.”
Kipnis, who joined the School of Medicine faculty in July as a BJC Investigator, is highly regarded for his groundbreaking work in neuroimmunology. In 2015, his lab discovered a network of vessels that drains fluid, immune cells and small molecules from the brain into the lymph nodes, for the first time demonstrating a direct physical connection between the brain and the immune system.
“It has long been known that every neurological disease has an immune component to it, and the assumption was that it was detrimental,” said Kipnis, who is also a professor of pathology and immunology, of neurology, of neurosurgery and of neuroscience. “But the immune system exists to protect and heal the body, not to destroy it. We want to know yet whether immune responses associated with neurological diseases indeed are beneficial – helping to prop up and possibly repair damaged neurons – or whether they are an underlying cause of illness. Our new center, through collaborations with numerous clinical and basic science departments, will cultivate and bring together scientists who want to be at the forefront of neuroimmunology and help answer such questions that could lead to entirely new approaches for treating diseases of the brain.”
The School of Medicine, with its exceptional research strengths in neuroscience and immunology, plus broad and deep expertise in teasing apart the underlying molecular contributions to numerous neurological conditions linked to immune and inflammatory dysfunction – such as Alzheimer’s disease, pain, itch, brain cancer, autism, and sleep disorders – provides an unparalleled environment for the center. The new center also will be able to draw upon the exceptional expertise found in the School of Medicine’s McDonnell Genome Institute to investigate genetic and genomic components of neuroimmunology.
“It is clear that inflammation plays an important role in Alzheimer’s disease and other neurodegenerative diseases,” said David Holtzman, MD, the Andrew B. and Gretchen P. Jones Professor and head of the Department of Neurology. “It will be important to better understand the details of this interaction as it may provide new innovative treatment approaches. This center will play an important role in supporting basic research to investigate how altering the immune system affects brain health and disease.”
The new center is supported by the Departments of Neurology, of Neurosurgery, of Neuroscience and of Pathology and Immunology. Its current leadership team includes Kipnis, Holtzman, and Marco Colonna, MD, the Robert Rock Belliveau Professor of Pathology and Immunology. Holtzman and Colonna have uncovered intriguing links between inflammation and Alzheimer’s disease. As the center grows and evolves, more experts will be added to the leadership team.
“Jony comes at a time of tremendous growth of our neurosciences and world-class immunology programs,” said Richard Cote, MD, the Edward Mallinckrodt Professor and head of the Department of Pathology and Immunology. “Already a leader, he will be a key part of building one of the great neuroimmunology programs in the world. As we face growing challenges in aging and neurodegenerative disease, we expect that fundamental approaches to these and other diseases of the brain will emanate from the BIG Center and the collaborations that will be enriched through the center.”
The center will be a highly interactive and collaborative hub for scientists from all disciplines and backgrounds interested in understanding how the relationship between the brain and the immune system can be manipulated to treat neurological diseases. It will offer a seminar series, workshops to help establish collaborative projects, grant-brewing sessions and journal clubs.
“Mentoring junior faculty is a passion of mine, and I hope that the center will be a greenhouse for new investigators and newcomers in the field,” Kipnis said. “We are planning to seek additional funding for exceptional projects in neuroimmunology and glia biology, with a goal to develop program projects and a neuroimmunology training program.
“Our knowledge linking the brain and the immune system is still in its infancy,” Kipnis continued. “We have much to explore, and the field is wide open. Given the exceptional strengths of clinical and basic neuroscience and immunology here, there is no better place to explore this new field of neuroimmunology than at Washington University. I look forward to working with many tremendous colleagues here and establishing new collaborations throughout the school and the university to push the boundaries of neuroimmunology and glia research to the next frontier.”







