$11.9 million from NIH funds glaucoma study
Researchers to evaluate effectiveness of earlier efforts to prevent, delay blinding eye disease
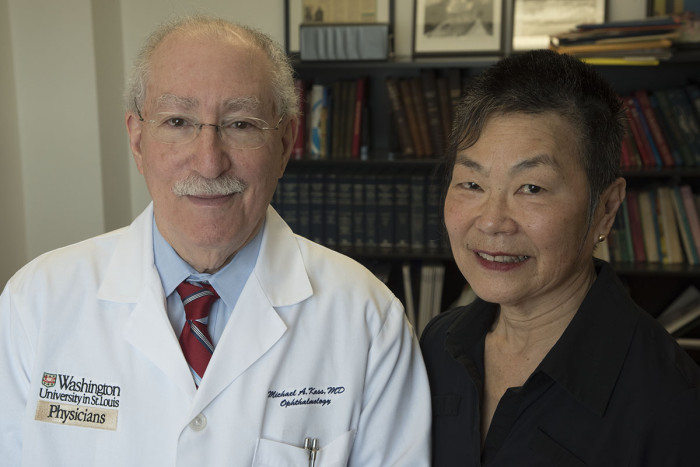
 Robert Boston
Robert BostonMichael A. Kass, MD, will lead a nationwide study to determine whether efforts to prevent or delay the onset of glaucoma have been effective over the course of two decades.

Researchers at Washington University School of Medicine in St. Louis have received four grants totaling $11.9 million from the National Eye Institute at the National Institutes of Health (NIH) to lead a nationwide study to determine whether efforts to prevent or delay the onset of glaucoma have been effective over the course of two decades. The new study is a follow-up to research led by the same Washington University scientists in the 1990s.
That research, the Ocular Hypertension Treatment Study, was conducted at 22 clinical sites in the United States and followed 1,636 subjects ages 40-80. Now, 20 years later, the same researchers are following up with the same subjects to see how their original conclusions have held up.
“We are going back to look at the same group of patients,” said Michael A. Kass, MD, lead investigator of the original study. “This is a landmark study because there just aren’t many 20-year studies conducted in vision research. We will conduct eye examinations to learn how many have developed glaucoma and, if so, how severe it is.”
All of the patients in the original study had elevated pressure in the eye, called ocular hypertension, but during the first phase of the study, only half were treated with pressure-lowering eye drops.
The researchers eventually found that patients at the highest risk for glaucoma needed to be treated — such as those who had elevated eye pressure and other symptoms including thin corneas. But they concluded that those with only elevated pressure should be monitored carefully but not necessarily treated.
Kass, a professor of ophthalmology and visual sciences, explained that a goal of the follow-up study is to create a model to allow clinicians to distinguish more clearly the patients at risk for rapidly progressing to glaucoma from those likely to progress more slowly.
In addition to running a clinical site in St. Louis, Washington University researchers again will oversee the national study.
“We’ll retrieve information about the vision of original patients in the study, or if they have passed away, we’ll attempt to retrieve their medical records,” said principal investigator Mae O. Gordon, PhD, professor of ophthalmology and visual sciences and of biostatistics.
In addition to finding that it wasn’t essential to lower eye pressure with drops unless patients also had other risk factors, the original study also showed that in African-American patients, lowering eye pressure with drops often didn’t prevent glaucoma.
Glaucoma is the leading cause of blindness in African-Americans, whose rate of blindness is four to six times higher than that of Caucasian patients.
The original study found that African-American patients who received pressure-lowering drops were about twice as likely to develop glaucoma as Caucasian patients treated with the drops. And the likelihood of glaucoma in African-American patients who didn’t get treatment was higher still. Those patients will be a particular focus of the new study.
“We have no way of knowing what the additional data will show,” Kass said. “But one thing we hope to learn is what happened with African-American patients at risk for glaucoma. We know many developed the disease, but we want to know how their disease progressed. Did treatment help preserve at least some of their vision?”






